Although vaccine interests are shielded from liability, in the United States, the Court of Justice of the European Union on 21 June 2017 still recognized causation when a healthy Mr. W received hepatitis B vaccine injections on 3 occasions (i.e. December 1998, January 1999, and July 1999). In August 1999 physical problems began to manifest, leading to an MS diagnosis in November 2000. In January 2001 Mr. W could no longer work and became functionally disabled at 90%, requiring around the clock care until dying in October 2011. Regarding causation, the court noted that when emerging data indicates an occurrence is not isolated then proof of vaccine harm can be established:
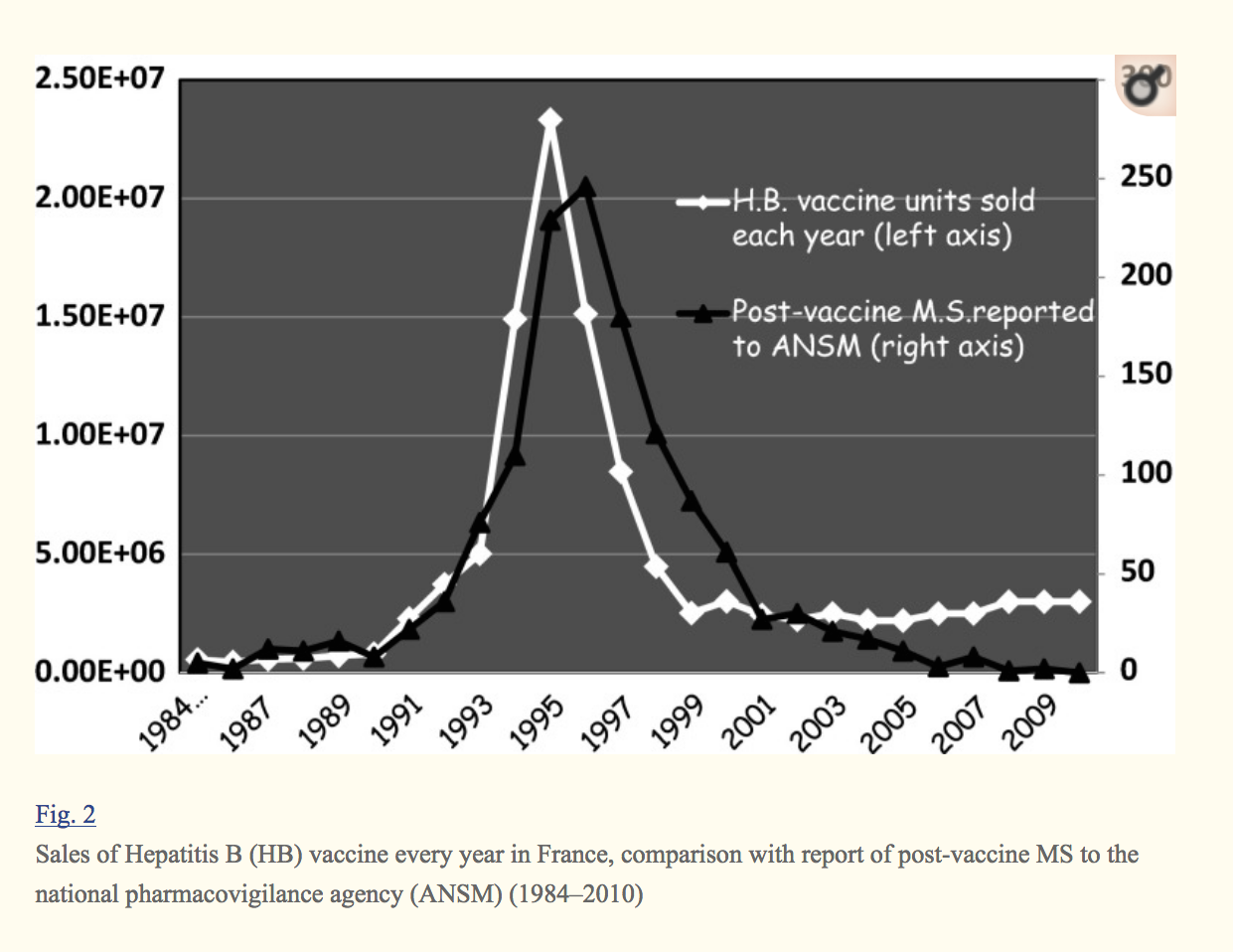
“The figures available in France thus show a definite statistical signal in favor of a causal link between the HB vaccine event and the apparition of MS with a maximum correlation in the 2 years following immunization.”
Le Houézec, D. (2014). Evolution of multiple sclerosis in France since the beginning of hepatitis B vaccination. Immunologic Research, 60(2-3), 219–225. http://doi.org/10.1007/s12026-014-8574-4
The temporal proximity between the administering of a vaccine and the occurrence of a disease, the lack of personal and familial history of the person vaccinated and the existence of a significant number of reported
cases of the disease occurring following such vaccines being administered may, where applicable, constitute sufficient evidence to make out such proof. (Judgment in Case C-621/15 N.W and others-v- Sanofi Pasteur MSD and Others, 2017)
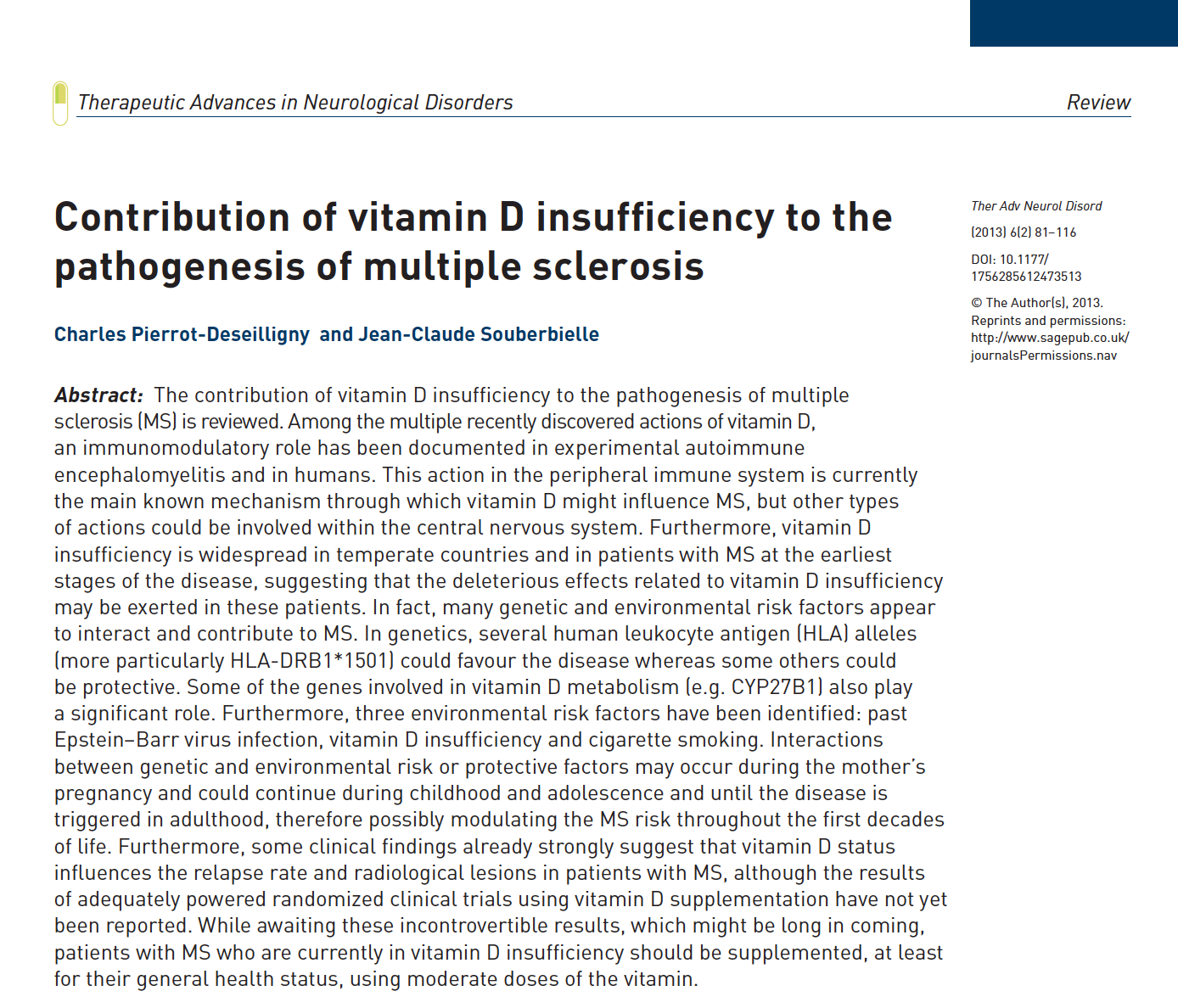
There is also evidence pointing to the involvement of cytokine Th17 in the pathogenesis of both hepatitis B and MS (Passos, Sato, Becker, & Fujihara, 2016; Liu et al., 2017). The modulation of Th17 occurs largely in the lungs and gastrointestinal tract. This is of interest nutritionally since high dietary salt intake increases Th17 differentiation (Passos et al, 2016, p. 3). This means reducing salt intake may be protective in those with MS. Another potential risk factor in MS is vitamin D deficiency. This is noteworthy because preliminary data shows vitamin D can down-regulate the expression of inflammatory Th17 cell-related cytokines (Jafarzadeh et al., 2018).
References:
Comenge, Y., & Girard, M. (2006). Multiple sclerosis and hepatitis B vaccination: adding the credibility of molecular biology to an unusual level of clinical and epidemiological evidence. Med Hypotheses, 66(1), 84-86. doi:10.1016/j.mehy.2005.08.012
Le Houézec, D. (2014). Evolution of multiple sclerosis in France since the beginning of hepatitis B vaccination. Immunologic Research, 60(2-3), 219–225. http://doi.org/10.1007/s12026-014-8574-4
Jafarzadeh, A., Azizi, S. V., Arabi, Z., Ahangar-Parvin, R., Mohammadi-Kordkhayli, M., Larussa, T., . . . Nemati, M. (2018). Vitamin D down-regulates the expression of some Th17 cell-related cytokines, key inflammatory chemokines, and chemokine receptors in experimental autoimmune encephalomyelitis. Nutr Neurosci, 1-13. doi:10.1080/1028415x.2018.1436237
Liu, Y., Li, L., Liu, J., She, W. M., Shi, J. M., Li, J., . . . Jiang, W. (2017). Activated hepatic stellate cells directly induce pathogenic Th17 cells in chronic hepatitis B virus infection. Exp Cell Res, 359(1), 129-137. doi:10.1016/j.yexcr.2017.08.001
Passos, G. R. D., Sato, D. K., Becker, J., & Fujihara, K. (2016). Th17 Cells Pathways in Multiple Sclerosis and Neuromyelitis Optica Spectrum Disorders: Pathophysiological and Therapeutic Implications. Mediators of Inflammation, 2016, 11. doi:10.1155/2016/5314541

